This is a div block with a Webflow interaction that will be triggered when the heading is in the view.
Modernize your cloud. Maximize business impact.
Small and mid-sized businesses (SMBs) in the healthcare sector are increasingly turning to cloud solutions to streamline operations, improve patient care, and reduce infrastructure costs. In fact, a recent study revealed that 70% of healthcare organizations have adopted cloud computing solutions, with another 20% planning to migrate within the next two years, indicating a 90% adoption rate by the end of 2025.
However, with the shift to digital platforms comes the critical responsibility of maintaining compliance with the Health Insurance Portability and Accountability Act (HIPAA). It involves selecting cloud providers that meet HIPAA requirements and implementing the right safeguards to protect sensitive patient data.
In this blog, we will look at how healthcare SMBs can stay HIPAA-compliant in the cloud, address their specific challenges, and explore how cloud solutions can help ensure both security and scalability for their systems.
Why HIPAA compliance is essential for cloud computing in healthcare
With the rise of cloud adoption, healthcare SMBs must ensure they meet HIPAA standards to protect data and avoid legal complications. Here are three key reasons why HIPAA compliance is so important in cloud computing for healthcare:
- Safeguarding electronic Protected Health Information (ePHI): HIPAA regulations require healthcare organizations to protect sensitive patient data, ensuring confidentiality and security. Cloud providers offering HIPAA-compliant services implement strong encryption methods and other security measures to prevent unauthorized access to ePHI.
- Mitigating risks of data breaches: Healthcare organizations are prime targets for cyberattacks, and data breaches can result in significant financial penalties and loss of trust. HIPAA-compliant cloud solutions provide advanced security features such as multi-factor authentication, secure data storage, and regular audits to mitigate these risks and prevent unauthorized access to patient data.
- Ensuring privacy and security of patient data: HIPAA ensures overall privacy and security beyond just ePHI protection. Cloud environments that comply with HIPAA standards implement safeguards that protect patient data both at rest and in transit, ensuring that healthcare organizations meet privacy requirements and provide patients with the peace of mind they deserve.
By maintaining HIPAA compliance in the cloud, healthcare organizations can also build trust with patients, safeguard valuable data, and streamline their operations.
Benefits of cloud computing for healthcare
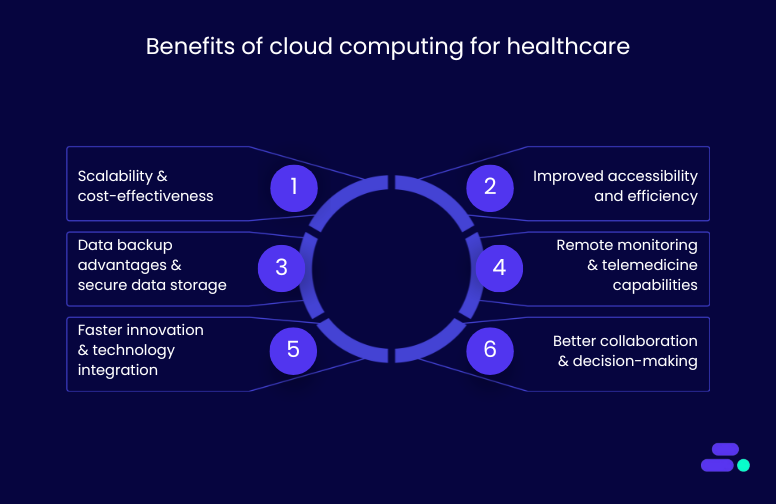
Cloud computing is reshaping the healthcare landscape, providing significant advantages that enhance service delivery, operational efficiency, and patient care. Here are some key benefits healthcare organizations can experience by adopting cloud solutions:
- Scalability and cost-effectiveness: Cloud computing allows healthcare organizations to adjust their infrastructure as needed, reducing the need for expensive hardware investments and offering pay-as-you-go models, making it ideal for SMBs with fluctuating demands.
- Improved accessibility and efficiency: Cloud-based systems enable healthcare teams to securely access, streamlining communication and speeding up diagnosis and treatment decisions. Administrative tasks also become more efficient, allowing healthcare professionals to focus on patient care.
- Reliable data backup and secure storage: Cloud computing provides backup solutions that ensure patient data is securely stored and easily recoverable in case of system failure or disaster, ensuring minimal downtime and business continuity.
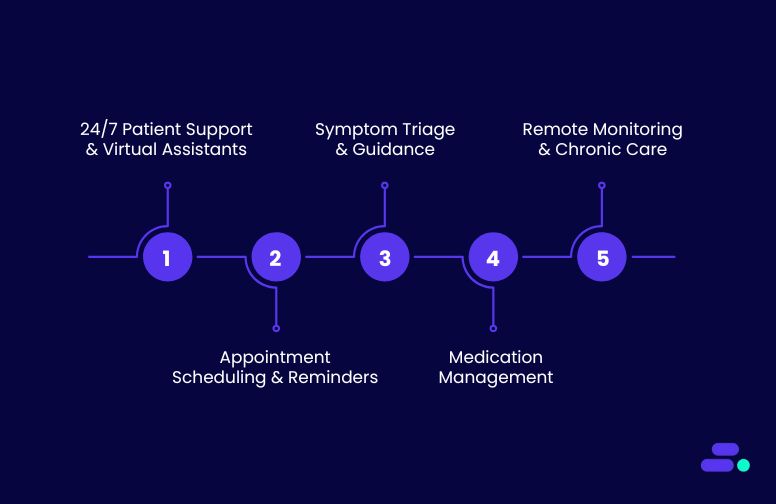
- Remote monitoring and telemedicine capabilities: Cloud platforms facilitate remote patient monitoring and telemedicine, allowing healthcare providers to offer care to patients in underserved or remote areas, thus improving access and patient outcomes.
- Faster innovation and technology integration: Cloud infrastructure enables healthcare organizations to quickly adopt new technologies like artificial intelligence (AI) and machine learning (ML), enhancing decision-making and enabling personalized care by efficiently analyzing large patient data sets.
Cloud-native innovations such as serverless computing and container orchestration (e.g., AWS Lambda and Amazon EKS) enable SMBs to improve compliance and scalability simultaneously, reducing operational complexity and risk. - Better collaboration and Decision-making: With cloud computing, real-time data sharing improves collaboration among healthcare teams across locations, ensuring decisions are based on the most current information and fostering more effective teamwork.
By using cloud computing, healthcare providers can improve their operational efficiency, reduce costs, and offer better, more accessible care to their patients.
HIPAA compliance requirements in cloud computing
Cloud computing is transforming healthcare by improving service quality, boosting operational efficiency, and enabling better patient outcomes. Below are the main HIPAA compliance factors to focus on:
1. Business associate agreements (BAAs) with cloud service providers (CSPs)
A Business Associate Agreement (BAA) is a legally binding contract between healthcare organizations and their cloud service providers (CSPs). The BAA outlines the provider’s responsibility to protect PHI (Protected Health Information) and comply with HIPAA regulations. Without a signed BAA, healthcare organizations cannot ensure that their CSP is following the necessary security and privacy protocols.
2. Ensuring data encryption at rest and in transit
To maintain HIPAA compliance, healthcare SMBs must ensure that Protected Health Information (PHI) is encrypted both at rest (when stored on cloud servers) and in transit (during transmission).
- Data at rest: PHI must be encrypted when stored on cloud servers to prevent unauthorized access in case of a breach.
- Data in transit: Encryption is also required when PHI is transmitted between devices and the cloud to protect against data interception during transit.
Encryption standards such as AES-256 are commonly used to meet HIPAA’s stringent data protection requirements.
3. Implementation of access controls and audit logging
To ensure HIPAA compliance, healthcare SMBs must implement access controls that limit PHI access to authorized personnel based on their roles (RBAC).
- Access controls: Only authorized personnel should have access to PHI. Role-based access control (RBAC) helps ensure that employees can only access the data necessary for their specific role.
- Audit logging: Cloud systems must include comprehensive audit logs that track all access to PHI, documenting who accessed data, when, and why. These logs are crucial for security audits and identifying unauthorized access.
4. Regular security risk assessments
Healthcare SMBs should perform regular security risk assessments to identify vulnerabilities in their cloud infrastructure.
- Evaluate cloud providers' security practices: Conduct penetration testing and ensure an effective disaster recovery plan to help mitigate threats and maintain HIPAA compliance.
- Ensure an efficient disaster recovery plan: The risk assessments include evaluating the cloud service provider’s security practices, conducting penetration testing, and ensuring their disaster recovery plan is efficient.
By regularly assessing security, organizations can mitigate potential threats and maintain HIPAA compliance.
5. Data backup and disaster recovery
Cloud providers must offer reliable data backup and disaster recovery options to protect patient data from loss. Healthcare organizations should ensure that backup solutions meet HIPAA standards, such as geographically dispersed storage for redundancy and quick data recovery. In case of a system failure or breach, quick recovery is essential to minimize downtime and maintain service continuity.
6. Vendor management and third-party audits
Healthcare organizations must ensure that their cloud service providers and any third-party vendors follow HIPAA guidelines. Regular third-party audits should be conducted to verify that CSPs comply with HIPAA security and privacy standards. Organizations should work with their CSPs to address audit findings promptly and implement necessary improvements.
Addressing these areas helps mitigate risks associated with cloud adoption, enabling healthcare organizations to meet regulatory standards and continue delivering high-quality care.
Also Read: Building HIPAA-compliant applications on the AWS cloud.
To meet these compliance requirements, healthcare SMBs need to implement proactive strategies that protect patient data and align with HIPAA regulations.
Strategies for maintaining HIPAA compliance in the cloud

Healthcare organizations—especially SMBs—must adopt proactive and structured strategies to meet HIPAA requirements while leveraging the benefits of cloud computing. These strategies help protect sensitive patient data and maintain regulatory alignment across cloud environments.
- Conduct regular risk assessments: Identify vulnerabilities across all digital systems, including cloud platforms. Evaluate how electronic Protected Health Information (ePHI) is stored, accessed, and transmitted. Use risk assessment insights to strengthen internal policies and address compliance gaps.
- Develop clear cybersecurity and compliance policies: Outline roles, responsibilities, and response plans in the event of a breach. Policies should align with HIPAA rules and be regularly updated to reflect evolving cloud practices and threat landscapes.
- Implement efficient technical safeguards: Use firewalls, intrusion detection systems, and end-to-end encryption to secure data both at rest and in transit. Ensure automatic data backups and redundancy systems are in place for data recovery.
Adopting Infrastructure as Code (IaC) tools like Terraform or AWS CloudFormation allows SMBs to automate security policy enforcement and maintain consistent, auditable configurations aligned with HIPAA requirements. - Establish and maintain access control protocols: Adopt role-based access, strong password requirements, and multi-factor authentication. Limit ePHI access to only those who need it and track access through detailed audit logs.
- Ensure CSP signs and complies with a business associate agreement (BAA): This agreement legally binds the cloud provider to uphold HIPAA security standards. It’s a non-negotiable element to use any third-party service to handle ePHI.
- Continuously monitor compliance and security measures: Regularly review system activity logs and CSP practices to confirm adherence to HIPAA standards. Leverage cloud-native monitoring tools for real-time alerts and policy enforcement.
- Train staff regularly on HIPAA best practices: Human error remains a leading cause of data breaches. Conduct frequent training sessions to keep teams informed on compliance policies, security hygiene, and breach response procedures.
By integrating these strategies, healthcare SMBs can confidently move forward in their cloud adoption journey while upholding the trust and safety of their patient data.
Choosing a HIPAA-compliant cloud service provider
Selecting the right cloud service provider (CSP) is critical for healthcare organizations looking to maintain HIPAA compliance. A compliant CSP should not only offer secure infrastructure but also demonstrate a clear understanding of HIPAA’s specific requirements for ePHI.
- Evaluate the CSP’s compliance certifications and track record: Look for providers that offer documented proof of compliance, such as HITRUST CSF, ISO/IEC 27001, or SOC 2 Type II. A strong compliance posture indicates the provider is prepared to handle sensitive healthcare data responsibly.
- Verify their willingness to sign a Business Associate Agreement (BAA): Under HIPAA, any third-party that handles ePHI is considered a business associate. A CSP must agree to sign a BAA, legally committing to uphold HIPAA security and privacy requirements. Without this agreement, working with the provider is non-compliant.
- Assess security features tailored for healthcare data: Choose CSPs that provide built-in encryption (at rest and in transit), detailed audit logging, role-based access controls, and real-time monitoring. These tools help healthcare SMBs meet HIPAA’s technical safeguard requirements.
- Review the provider’s shared responsibility model: Understand which aspects of security and compliance are managed by the CSP and which are the responsibility of the customer. A transparent shared responsibility model avoids compliance gaps and misconfigurations.
- Evaluate support and incident response capabilities: Choose a provider that offers 24/7 technical support, a clear escalation path for security incidents, and defined recovery time objectives. A timely response can minimize the impact of breaches or service disruptions.
- Consider the CSP’s experience in healthcare: A provider familiar with healthcare clients will be better equipped to meet HIPAA expectations. Look for case studies or client references that demonstrate success in the healthcare space.
By thoroughly vetting potential cloud providers through these criteria, healthcare organizations can make informed decisions that reduce risk and ensure compliance from the ground up.
Cloudtech helps your business achieve and maintain HIPAA compliance in the cloud, without compromising on performance or scalability. With Cloudtech, you get expert guidance, ongoing compliance support, and a secure infrastructure built to handle sensitive patient data.
Challenges and risks of cloud computing in healthcare
While cloud computing offers numerous benefits, it also presents specific challenges that healthcare organizations must address to stay compliant and secure.
- Management of shared infrastructure and potential compliance issues: Cloud environments often operate on a shared infrastructure model, where multiple clients access common resources. Without strict isolation and proper configuration, this shared model can increase the risk of unauthorized access or compliance violations.
- Handling security and privacy concerns effectively: Healthcare data is a prime target for cyberattacks. Ensuring encryption, access controls, and real-time monitoring is essential. However, gaps in internal policies or misconfigurations can lead to breaches, even with advanced cloud tools in place.
- Dealing with jurisdictional issues related to cloud data storage: When cloud providers store data across multiple geographic locations, regulatory conflicts may arise. Data residency laws vary by country and can impact how patient information is stored, accessed, and transferred. Healthcare organizations must ensure their provider aligns with regional legal requirements.
- Maintaining visibility and control over cloud resources: As services scale, it can become difficult for internal teams to maintain oversight of all assets, configurations, and user activity. Without proper governance, this lack of visibility can increase the risk of non-compliance and delayed incident response.
- Ensuring staff training and cloud literacy: Adopting cloud technology requires continuous training for IT and administrative staff. Misuse or misunderstanding of cloud tools can compromise security or lead to HIPAA violations, even with strong technical safeguards in place.
To overcome these challenges, healthcare organizations should follow best practices to ensure continuous HIPAA compliance and safeguard patient data.
Best practices for ensuring HIPAA compliance
Healthcare organizations using the cloud must follow proven practices to protect patient data and stay HIPAA compliant.
- Sign business associate agreements (BAAs): Ensure the cloud service provider signs a BAA, clearly defining responsibilities for handling ePHI and meeting HIPAA standards.
- Enforce access controls and monitor activity: Restrict access based on roles and monitor data activity through audit logs and alerts to catch and address unusual behavior early.
- Respond quickly to security incidents: Have a clear incident response plan to detect, contain, and report breaches promptly, following HIPAA’s Breach Notification Rule.
- Conduct regular risk assessments: Periodic reviews of the cloud setup help spot vulnerabilities and update safeguards to meet current HIPAA requirements.
- Train staff on HIPAA and cloud security: Educate employees on secure data handling and how to avoid common threats like phishing to reduce human error.
Conclusion
As healthcare organizations, particularly SMBs, move forward with digital transformation, ensuring HIPAA compliance in cloud computing is both a necessity and a strategic advantage. Protecting electronic protected health information (ePHI), reducing the risk of data breaches, and benefiting from scalable, cost-effective solutions are key advantages of HIPAA-compliant cloud services.
However, achieving compliance is not just about using the right technology; it requires a comprehensive strategy, the right partnerships, and continuous monitoring.
Looking for a reliable partner in HIPAA-compliant cloud solutions?
Cloudtech provides secure, scalable cloud infrastructure designed to meet HIPAA standards. With a focus on encryption and 24/7 support, Cloudtech helps organizations protect patient data while embracing the benefits of cloud technology.
FAQs
- What is HIPAA compliance in cloud computing?
HIPAA compliance in cloud computing ensures that cloud service providers (CSPs) and healthcare organizations adhere to strict regulations for protecting patient data, including electronic Protected Health Information (ePHI). This includes data encryption, secure storage, and ensuring privacy and security throughout the data lifecycle.
- How can healthcare organizations ensure their cloud service provider is HIPAA-compliant?
Healthcare organizations should ensure their cloud service provider signs a Business Associate Agreement (BAA), provides encryption methods (both at rest and in transit), and offers secure access controls, audit logging, and real-time monitoring to protect ePHI.
- What are the key benefits of using cloud computing for healthcare organizations?
Cloud computing provides healthcare organizations with scalability, improved accessibility, cost-effectiveness, enhanced data backup, and disaster recovery solutions. Additionally, it supports remote monitoring and telemedicine, facilitating more accessible patient care and improved operational efficiency.
- What are the consequences of non-compliance with HIPAA regulations in cloud computing?
Non-compliance with HIPAA regulations can lead to severe penalties, including hefty fines and damage to an organization’s reputation. It can also result in unauthorized access to sensitive patient data, leading to breaches of patient privacy and trust.
- What should be included in a HIPAA-compliant cloud security strategy?
A HIPAA-compliant cloud security strategy should include regular risk assessments, encryption of ePHI, access control mechanisms, audit logging, a disaster recovery plan, and ongoing staff training. Additionally, healthcare organizations should ensure their cloud provider meets all HIPAA technical safeguards and legal obligations.

Get started on your cloud modernization journey today!
Let Cloudtech build a modern AWS infrastructure that’s right for your business.